Diabetes, Types of Diabetes, Risk factors, Prevention and Management, Symptoms and Treatment by Medications
What is Diabetes?
Diabetes is a chronic (long-lasting) health condition that controls sugar level in your blood after eating foods. Foods, we eat and drink, are converted into sugar (glucose) and released into bloodstream. Our pancreas releases insulin when our blood sugar levels become high and insulin helps blood sugar enter the body’s cells for use as energy.
If people have diabetes, their body doesn’t produce enough insulin or if produced, it is not used as well as it should be. Cells may stop responding to insulin. Therefore, blood sugar levels become very high in bloodstream. After long time, this health condition can lead to different serious health problems, such as heart disease, vision loss, kidney disease, etc.
Types of Diabetes
There are three main types of diabetes: type 1, type 2 and gestational diabetes (diabetes while pregnant).
What is Type 1 Diabetes?
An autoimmune reaction (the body attacks itself by mistake) causes type 1 diabetes. This reaction prevents your body to produce insulin. About 5-10% of the diabetic people have type 1 diabetes. The children, teens, and young adults are usually diagnosed with type 1 diabetes. There is no treatment or method to cure it or prevent it, but the people with type 1 diabetes require to take insulin every day to survive.
Type 2 Diabetes
Your body doesn’t produce enough insulin or can not use insulin well. As a result, blood sugar level becomes higher than normal levels. It develops over many years. About 90-95% of people with diabetes have type 2.
Gestational Diabetes
Some women get diabetes when they are pregnant although they never had diabetes before pregnancy. It is called gestational diabetes. After the birth of baby, gestational diabetes normally goes away, but mother may get type 2 diabetes later in life. Baby could be at higher health risk. They may have obesity as a child or teen and develop type 2 diabetes later in life. Therefore, gestational diabetes is strictly controlled during pregnancy before the birth of baby.
Prediabetes
Prediabetes condition is the primary state of the body before developing type 2 diabetes. People with prediabetes condition have blood sugar levels higher than normal, but it is not high enough for a type 2 diabetes diagnosis.
Risk:
Prediabetes increases the risk of type 2 diabetes, heart disease, and stroke.
Prevention of prediabetes
Lifestyle change can help people to prevent developing type 2 diabetes and reverse it.
Risk Factors of Diabetes
Different types of diabetes have different risk factors (Ref.: CDC, 2023).
Type 1 Diabetes
Although the risk factors for type 1 diabetes are not very clear, but the following factors are presumed to be responsible:
- Family history: Having a parent, brother, or sister with type 1 diabetes.
- Age: You can get type 1 diabetes at any age, but it usually develops in children, teens, or young adults.
Type 2 Diabetes
Risk factors for type 2 diabetes are as below (Ref.: CDC, 2023):
- Prediabetes.
- Overweight.
- Age of 45 years or older.
- Family history of type 2 diabetes.
- Are physically active less than 3 times a week.
- Have ever had gestational diabetes (diabetes during pregnancy) or given birth to a baby who weighed over 9 pounds.
- Are an African American, Hispanic or Latino, American Indian, or Alaska Native person. Some Pacific Islanders and Asian American people are also at higher risk.
- If you have non-alcoholic fatty liver disease you may also be at risk for type 2 diabetes.
Risk Factors of Gestational Diabetes (Ref.: CDC, 2023):
- Had gestational diabetes during a previous pregnancy.
- Have given birth to a baby who weighed over 9 pounds.
- Are overweight.
- Are more than 25 years old.
- Have a family history of type 2 diabetes.
- Have a hormone disorder called polycystic ovary syndrome (PCOS).
- Are an African American, Hispanic or Latino, American Indian, Alaska Native, Native Hawaiian, or Pacific Islander person.
Prevention of Gestational Diabetes
Women can prevent gestational diabetes before they become pregnant by changing their lifestyle options. Most important lifestyle changes are as below:
- Losing weight if you’re overweight,
- Eating a healthy diet,
- Practising regular physical activity.
How to Prevent or Manage Diabetes
Diabetes can’t be cured permanently, but it can be managed by following some lifestyles choices and medications as below:
- Losing weight,
- Eating healthy food,
- Be active/Physical activity,
- Take medicine as prescribed.
Symptoms of Diabetes
If you have any of the following symptoms, you must consult with doctor, and get your blood sugar tested to confirm your diabetes or prediabetes conditions:
- Frequent urination, often at night
- Very thirsty
- Weight loss without trying
- Getting very hungry
- Having blurry vision
- Having numb or tingling hands or feet
- Feeling very tired
- Having very dry skin
- Having sores that heal slowly
- Having more infections than usual
Symptoms of Type 1 Diabetes
- People with type 1 diabetes may also have nausea, vomiting, or stomach pains.
- Symptoms can develop in just a few weeks or months and can be severe.
Symptoms of Type 2 Diabetes
- It often takes several years to develop type 2 diabetes symptoms.
- Sometimes, symptoms of some people are not noticeable at all.
- It is difficult to notice symptoms for some people.
- Therefore, it is better to understand the risk factors for type 2 diabetes.
- Consult your doctor if you notice any symptoms.
Symptoms of Gestational Diabetes
- Gestational Diabetes normally doesn’t show any symptoms.
- Doctor test you for gestational diabetes between 24 and 28 weeks of pregnancy.
- You must change lifestyle options to prevent gestational diabetes, protect your health and your baby’s health.
Treatment of Type 2 Diabetes by Medications
Different types and classes of medications are available in the pharmacies that are used by people with diabetes to lower blood sugar. These medications work in different ways, but their main goals are to lower blood glucose/sugar level. Some of them are taken orally, while others are injected. Besides insulin, there are some medications widely used by diabetics. We will discuss some of the more commonly used medicines as below:
- Metformin
- DPP-4 inhibitors
- GLP-1 and dual GLP-1/GIP receptor agonists
- SGLT2 Inhibitors
Metformin
Metformin (Glucophage) is a well-known medication for type-2 diabetes patients and it is called a biguanide medication. It mainly decreases the amount of glucose produced by the liver leading to lowering of blood glucose levels. Metformin makes muscle tissue more sensitive to insulin and also helps lower blood glucose levels. Therefore, glucose becomes available for energy production. Metformin is widely taken by many people with type-2 diabetes and even by people with prediabetes. It is prescribed as a first-line therapy to manage type 2 diabetes.
Side effects
Although metformin may have a side effect like diarrhea, however, consumption of this drug with food may improve it.
Limitations
Metformin does not help weight loss. Sometimes, metformin may not be sufficient for some people as time goes on. This medication is not fully effective for some people or some people can’t manage type-2 diabetes by taking only metformin.
Combination therapy
The people, taking metformin, may need additional medication for their diabetes management. They can take additional oral or injectable medications in addition to metformin. The drugs of different groups act in different ways to lower blood glucose levels. Therefore, the medications from different groups may be used together for individual diabetes management. This is called as combination therapy which is, sometimes, more effective for diabetes management and reduce the diabetes-related complications, such as heart disease or chronic kidney disease. However, you should still continue your diet management and physical activity. Monitor the blood glucose levels after taking the combination therapy. Your healthcare provider will prescribe you the combination of medicines that work best for you and your lifestyle, and provide you the ease of diabetes management.
DPP-4 Inhibitors
DPP-4 inhibitors are the useful medications for the diabetic people, which help improve A1C (a measure of average blood glucose levels over 2-3 months), but they don’t cause hypoglycemia (low blood glucose). The main function of this medication is to prevent the breakdown of naturally occurring hormones in the body, GLP-1 and GIP, which reduce blood glucose levels in the body. But these hormones are broken down very quickly. DPP-4 inhibitors interfere in the process of breaking down the GLP-1 and GIP, and therefore, these hormones remain active in the body for longer time, and help reduce blood glucose levels only when they are elevated. The diabetic people taking DPP-4 inhibitors do not have the possibility of getting weight gain, and they can nicely tolerate these medications.
DPP-4 inhibitors currently available in the market are as below:
- Alogliptin (Nesina)
- Linagliptin (Tradjenta)
- Saxagliptin (Onglyza)
- Sitagliptin (Januvia)
GLP-1 and Dual GLP-1/GIP Receptor Agonists
GLP-1 medications lower the blood glucose levels by the following mechanisms. They increase insulin production, decrease glucagon release, keep food in stomach longer than normal time and reduce the feeling of hunger. Thus, these medications keep the blood sugar level under control and provide the benefit of weight loss.
The medications GLP-1 and dual GLP-1/GIP receptor agonists are very beneficial for the blood glucose management of the type-2 diabetic patients. These medications demonstrate almost similar effects to the GLP-1 and GIP produced in the body, but these drugs are resistant to being broken down by the DPP-4 enzyme. Some of these drugs are useful to prevent heart disease.
All of the medications are used as injections except semaglutide (Rybelsus), which is taken orally once daily. It is an oral formulation of semaglutide. Tirzepatide (Mounjaro) is a dual GLP-1/GIP receptor agonist currently available on the market. The list of all drugs is as below:
- Dulaglutide (Trulicity)
- Exenatide (Byetta)
- Exenatide extended-release (Bydureon)
- Liraglutide (Victoza)
- Lixisenatide (Adlyxin)
- Injectable semaglutide (Ozempic)
- Tirzepatide (Mounjaro)
Side effects
The people taking these medications may experience some most common side effects, such as nausea and vomiting when they start taking these medications or increase the dose of medications. But these side effects normally go away after the consumers take time to adjust to the medications. The patients need to consult with the doctors who can balance the benefits and side effects of these medications.
SGLT2 Inhibitors
SGLT2 inhibitors is a new class of drugs that help to increase elimination of blood sugar into the urine by working on the kidneys. Sodium-glucose co-transporter 2 (SGLT2) works in the kidney to reabsorb glucose. SGLT2 inhibitors prevent this action and help to eliminate excess glucose in the urine. People can reduce blood glucose level by increasing the amount of glucose excreted in the urine. These medications are recommended for the people with type-2 diabetes who have high A1C levels. These drugs also help to reduce blood pressure (small decrease) and gain some weight loss.
The Food and Drug Administration (FDA) has approved the following SGLT2 inhibitors to treat type 2 diabetes:
- Bexagliflozin (Brenzavvy),
- Canagliflozin (Invokana),
- Dapagliflozin (Farxiga),
- Empagliflozin (Jardiance),
- Ertugliflozin (Steglatro)
Other benefits
SGLT2 inhibitors can benefit the people to reduce the heart disease, kidney disease, and heart failure. Therefore, the healthcare providers prescribe these medications for the people with type 2 diabetes who also have heart or kidney problems.
Side effects
The most common side effects observed in the people taking these drugs are genital yeast infections due to increased glucose levels in the urine. There is potential of some other side effects, such as urinary tract infections, constipation, and flu-like symptoms.
Reference
American Diabetes Association, 2023. What Are My Options for Type 2 Diabetes Medications? URL: https://diabetes.org/healthy-living/medication-treatments/oral-other-injectable-diabetes-medications. Date accessed on 16/05/2023.
CDC, 2023. Diabetes. Centers for Disease Control and Prevention. URL: https://www.cdc.gov/diabetes/basics/diabetes.html. Accessed on 22/05/2023.
Endocrineweb, 2023. URL: https://www.endocrineweb.com/conditions/type-2-diabetes/insulin-alternatives. Accessed on 16/05/2023.
Diabetic kidney disease: Use of metabolomics for early diagnosis
Dr Md Anawar Hossain
How Does Kidney Function?
Kidney filters wastes and extra water out of the blood to make urine. It also helps to control blood pressure and makes hormones for healthy body. If kidneys are damaged, they can’t filter blood, which can cause wastes to build up in the body and cause other health problems (NIDDK, 2022).
What is Diabetic Kidney Disease (DKD)?
Diabetic kidney disease (DKD) is an alarming public health issue (Abdelsattar et al., 2021). Diabetic kidney disease is one of the most prevalent comorbidities of diabetes mellitus and the leading cause of the end-stage renal disease (ESRD). DKD develops in approximately 40% of patients with diabetes worldwide (Alicic et al., 2017). DKD can increase in its prevalence reaching 44% by 2030 (Abdelsattar et al., 2021). It is also called chronic kidney disease (CKD), kidney disease of diabetes, or diabetic nephropathy.
Diabetes dangerously leads to the kidney disease causing about 1 out of 3 adults with diabetes to kidney disease (CDCP, 2019). DKD results from chronic exposure to hyperglycemia, caused by diabetes, leading to progressive alterations in kidney structure and function (NIDDK, 2022). The early development of DKD is clinically silent and when albuminuria is detected the lesions are often at advanced stages, leading to rapid kidney function decline resulting in the end-stage renal disease (Pereira et al., 2022). However, the majority of patients actually die from cardiovascular diseases and infections before needing kidney replacement therapy (Alicic et al., 2017).
Kidney Disease by Diabetes
The high concentration of blood sugar can damage the blood vessels of human kidney and ultimately damage kidney function. Many diabetic people also have high blood pressure, which can damage kidneys. If someone has diabetes for a longer time or if they have diabetes, high blood sugar and high blood pressure, they have more probability to develop kidney disease. People with diabetes are also more likely to develop kidney disease if they (1) smoke, (2) don’t follow diabetes eating plan, (3) eat foods high in salt, (4) are not active, (5) are overweight, (6) have heart disease, and (7) have a family history of kidney failure (NIDDK, 2022).
Diabetes causes metabolic changes leading to glomerular hypertrophy, glomerulosclerosis, and tubulointerstitial inflammation and fibrosis (Alicic et al., 2017).
Precaution and Monitoring
DKD progression can be arrested or substantially delayed if detected and addressed at early stages. A major limitation of current methods is the absence of albuminuria in non-albuminuric phenotypes of diabetic nephropathy, which becomes increasingly prevalent and lacks focused therapy (Pereira et al., 2022). The study of characteristic metabolic alterations of DKD can help to understand pathogenesis and identify new potential biomarkers and drug targets. Therefore, Abdelsattar et al. (2021) hypothesized that metabolic profiling of amino acids, acylcarnitines, and organic acids can be new biomarkers for the diagnosis of the early stages of DKD. Diabetes usually causes kidney damage slowly, over many years. Therefore, people can make plan and take initiative to prevent or delay kidney damage.
Kidney damage from diabetes can get worse over time. Maintaining blood sugar and blood pressure level under control can protect the kidneys and slow or prevent diabetes-related kidney disease. Medicines may be an important part of treatment plan as prescribed by healthcare professionals (NIDDK, 2022).
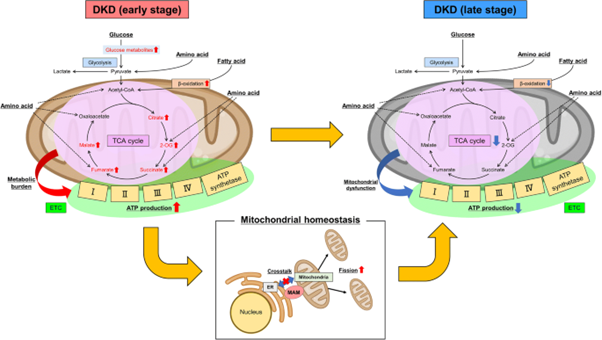
Metabolomics and Its Use to Identify Early Stage of Diabetic kidney disease
Metabolomics is one of the omics technologies that can detect metabolites in living organism. Metabolomics can determine complex metabolic networks in human body and give insight of several physiological or pathophysiological processes, that can identify the diseases’ unique metabolic signatures. Thus, metabolomics is a promising tool that can not only detect metabolites but also identify pre-disease states for the early clinical practice and treatment. Therefore, the use of metabolomics as a tool can identify the DKD metabolic signature of tubule interstitial lesions to diagnose or predict the time-course of DKD (Pereira et al., 2022).
DKD leads to increasing urinary albumin excretion with a rise in proteinuria and a drop in estimated glomerular filtration rate (eGFR) in the absence of other renal diseases (Abdelsattar et al., 2021). The albumin to creatinine ratio (ACR) can determine renal function. But the muscle mass and the physical activity can affect the ratio due to the variable creatinine excretion in male and female, and the equations such as the Modification of Diet in Renal Disease (MDRD) used for the estimation of GFR. There are several drawbacks to the use of urine albumin. Therefore, a suitable biomarker is needed to identify the renal function. Abdelsattar et al. (2021) reported that dodecanoylcarnitines C12, triglylcarnitine C5:1, and isovalerylcarnitine C5 were stronger predictors of albumin/creatinine ratio than HbA1c and suggested them as potential biomarkers for the diagnosis of the early stages of DKD.
References
Abdelsattar S., Kasemy Z.A., Elsayed M., Elrahem T.A., Zewain S.K., 2021. Targeted metabolomics as a tool for the diagnosis of kidney disease in Type II diabetes mellitus, British Journal of Biomedical Science, DOI: 10.1080/09674845.2021.1894705
Alicic R.Z., Rooney M.T., Tuttle K.R., 2017. Diabetic Kidney Disease Challenges, Progress, and Possibilities. Clin J Am Soc Nephrol. Vol. 12, 2032–2045.
Hasegawa S., Inagi R., 2021. Harnessing metabolomics to describe the pathophysiology underlying progression in diabetic kidney disease. Curr Diab Rep 21, 21. https://doi.org/10.1007/s11892-021-01390-8
Pereira P.R., Carrageta D.F., Oliveira P.F., Rodrigues A., Alves M.G., Monteiro M.P., 2022. Metabolomics as a tool for the early diagnosis and prognosis of diabetic kidney disease. Medicinal Research Reviews, Vol. 42 (4), 1518-1544.
NIDDK, 2022. Diabetic Kidney Disease. Link: https://www.niddk.nih.gov/health-information/diabetes/overview/preventing-problems/diabetic-kidney-disease. Accessed on 22/08/2022.
CDCP (Centers for Disease Control and Prevention), 2019. Chronic Kidney Disease in the United States, 2019. Atlanta, GA: US Department of Health and Human Services. Centers for Disease Control and Prevention; 2019.
