Dr Md Anawar Hossain
How Does Kidney Function?
Kidney filters wastes and extra water out of the blood to make urine. It also helps to control blood pressure and makes hormones for healthy body. If kidneys are damaged, they can’t filter blood, which can cause wastes to build up in the body and cause other health problems (NIDDK, 2022).
What is Diabetic Kidney Disease (DKD)?
Diabetic kidney disease (DKD) is an alarming public health issue (Abdelsattar et al., 2021). Diabetic kidney disease is one of the most prevalent comorbidities of diabetes mellitus and the leading cause of the end-stage renal disease (ESRD). DKD develops in approximately 40% of patients with diabetes worldwide (Alicic et al., 2017). DKD can increase in its prevalence reaching 44% by 2030 (Abdelsattar et al., 2021). It is also called chronic kidney disease (CKD), kidney disease of diabetes, or diabetic nephropathy.
Diabetes dangerously leads to the kidney disease causing about 1 out of 3 adults with diabetes to kidney disease (CDCP, 2019). DKD results from chronic exposure to hyperglycemia, caused by diabetes, leading to progressive alterations in kidney structure and function (NIDDK, 2022). The early development of DKD is clinically silent and when albuminuria is detected the lesions are often at advanced stages, leading to rapid kidney function decline resulting in the end-stage renal disease (Pereira et al., 2022). However, the majority of patients actually die from cardiovascular diseases and infections before needing kidney replacement therapy (Alicic et al., 2017).
Kidney Disease by Diabetes
The high concentration of blood sugar can damage the blood vessels of human kidney and ultimately damage kidney function. Many diabetic people also have high blood pressure, which can damage kidneys. If someone has diabetes for a longer time or if they have diabetes, high blood sugar and high blood pressure, they have more probability to develop kidney disease. People with diabetes are also more likely to develop kidney disease if they (1) smoke, (2) don’t follow diabetes eating plan, (3) eat foods high in salt, (4) are not active, (5) are overweight, (6) have heart disease, and (7) have a family history of kidney failure (NIDDK, 2022).
Diabetes causes metabolic changes leading to glomerular hypertrophy, glomerulosclerosis, and tubulointerstitial inflammation and fibrosis (Alicic et al., 2017).
Precaution and Monitoring
DKD progression can be arrested or substantially delayed if detected and addressed at early stages. A major limitation of current methods is the absence of albuminuria in non-albuminuric phenotypes of diabetic nephropathy, which becomes increasingly prevalent and lacks focused therapy (Pereira et al., 2022). The study of characteristic metabolic alterations of DKD can help to understand pathogenesis and identify new potential biomarkers and drug targets. Therefore, Abdelsattar et al. (2021) hypothesized that metabolic profiling of amino acids, acylcarnitines, and organic acids can be new biomarkers for the diagnosis of the early stages of DKD. Diabetes usually causes kidney damage slowly, over many years. Therefore, people can make plan and take initiative to prevent or delay kidney damage.
Kidney damage from diabetes can get worse over time. Maintaining blood sugar and blood pressure level under control can protect the kidneys and slow or prevent diabetes-related kidney disease. Medicines may be an important part of treatment plan as prescribed by healthcare professionals (NIDDK, 2022).
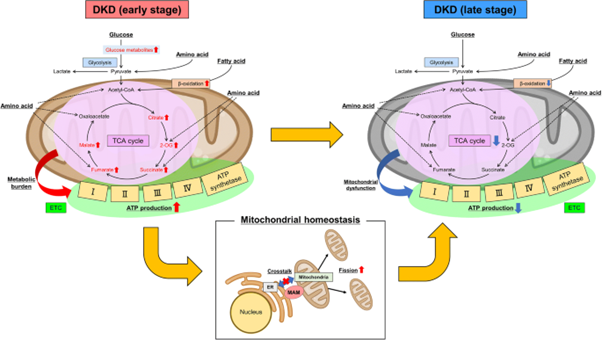
Metabolomics and Its Use to Identify Early Stage of Diabetic kidney disease (DKD)
Metabolomics is one of the omics technologies that can detect metabolites in living organism. Metabolomics can determine complex metabolic networks in human body and give insight of several physiological or pathophysiological processes, that can identify the diseases’ unique metabolic signatures. Thus, metabolomics is a promising tool that can not only detect metabolites but also identify pre-disease states for the early clinical practice and treatment. Therefore, the use of metabolomics as a tool can identify the DKD metabolic signature of tubule interstitial lesions to diagnose or predict the time-course of DKD (Pereira et al., 2022).
DKD leads to increasing urinary albumin excretion with a rise in proteinuria and a drop in estimated glomerular filtration rate (eGFR) in the absence of other renal diseases (Abdelsattar et al., 2021). The albumin to creatinine ratio (ACR) can determine renal function. But the muscle mass and the physical activity can affect the ratio due to the variable creatinine excretion in male and female, and the equations such as the Modification of Diet in Renal Disease (MDRD) used for the estimation of GFR. There are several drawbacks to the use of urine albumin. Therefore, a suitable biomarker is needed to identify the renal function. Abdelsattar et al. (2021) reported that dodecanoylcarnitines C12, triglylcarnitine C5:1, and isovalerylcarnitine C5 were stronger predictors of albumin/creatinine ratio than HbA1c and suggested them as potential biomarkers for the diagnosis of the early stages of DKD.
References
Abdelsattar S., Kasemy Z.A., Elsayed M., Elrahem T.A., Zewain S.K., 2021. Targeted metabolomics as a tool for the diagnosis of kidney disease in Type II diabetes mellitus, British Journal of Biomedical Science, DOI: 10.1080/09674845.2021.1894705
Alicic R.Z., Rooney M.T., Tuttle K.R., 2017. Diabetic Kidney Disease Challenges, Progress, and Possibilities. Clin J Am Soc Nephrol. Vol. 12, 2032–2045.
Hasegawa S., Inagi R., 2021. Harnessing metabolomics to describe the pathophysiology underlying progression in diabetic kidney disease. Curr Diab Rep 21, 21. https://doi.org/10.1007/s11892-021-01390-8
Pereira P.R., Carrageta D.F., Oliveira P.F., Rodrigues A., Alves M.G., Monteiro M.P., 2022. Metabolomics as a tool for the early diagnosis and prognosis of diabetic kidney disease. Medicinal Research Reviews, Vol. 42 (4), 1518-1544.
NIDDK, 2022. Diabetic Kidney Disease. Link: https://www.niddk.nih.gov/health-information/diabetes/overview/preventing-problems/diabetic-kidney-disease. Accessed on 22/08/2022.
CDCP (Centers for Disease Control and Prevention), 2019. Chronic Kidney Disease in the United States, 2019. Atlanta, GA: US Department of Health and Human Services. Centers for Disease Control and Prevention; 2019.